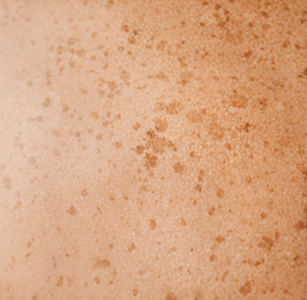
Understanding Hyperpigmentation










⬑ Darkened pigmentation from years of accumulated UV exposure









We're here to help you manage your skin concerns.
Solano F, “Melanins: Skin pigments and much more—types, structural models, biological functions, and formation routes.” New Journal of Science 2014 (2014): 1-28.
Passeron T et al., “Melasma pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and melasma treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Grimes PE et al., “Melasma: Etiologic and therapeutic considerations.” Archives of Dermatology 141, no. 1 (2005): 89-93.
Lim JT et al., “Sun protection and prevention of hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Boonchai W et al., “Post-inflammatory hyperpigmentation: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Sardana K et al., “Rebound pigmentation and its management in hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Handog EB et al., “Challenges in the management of hyperpigmentation: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Briganti S et al., “Melanin: What is it and how is it produced?” International Journal of Cosmetic Science 25, no. 6 (2003): 279-289.
Grimes PE et al., “Histologic changes in hyperpigmented skin.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Aldahan AS et al., “Topical treatments for melasma and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Alvarez OM et al., “Botanical extracts for skin lightening: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Draelos ZD et al., “Efficacy of natural ingredients in anti-pigmentation and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Nistico SP et al., “Efficacy of botanical formulations for managing hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Sivamani RK et al., “Natural alternatives for treating hyperpigmentation and skin inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Hassim Z et al., “Hormonal influences on hyperpigmentation: A comprehensive review.” International Journal of Women’s Dermatology 6, no. 2 (2020): 73-82.
Rodriguez CI et al., “Role of oxidative stress in hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Kraft JN et al., “The role of inflammation in hyperpigmentation and its management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Nistico SP et al., “Topical retinoids and inflammation: A review.” Dermatologic Therapy 34, no. 2 (2021): e14830.
Goldberg DJ et al., “Pigment-safe laser treatments for benign skin lesions.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in hyperpigmentation management.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Clearer Skin, Lasting Confidence
Painless, Plant-Tech Approach

⬑ Customised set of botanical formulations unique to you on every visit

Targets Pigmentation Root Cause


Limits Spread and Rebound Pigmentation


No Lifestyle Limitations


Lasting Results, Without Compromise


We're here to help you manage your skin concerns.
At Folke®, we address skin concerns at the root for lasting results. Our painless, non-invasive, customised plant-tech approach protects your skin and health, delivering visible, personalised improvements backed by over 20 years of expertise.
Briganti S et al., “Melanin: What is it and how is it produced?” International Journal of Cosmetic Science 25, no. 6 (2003): 279-289.
Solano F, “Melanins: Skin pigments and much more—types, structural models, biological functions, and formation routes.” New Journal of Science 2014 (2014): 1-28.
Lim JT et al., “Sun protection and prevention of hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Goldberg DJ et al., “Pigment-safe laser treatments for benign skin lesions.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Grimes PE et al., “Melasma: Etiologic and therapeutic considerations.” Archives of Dermatology 141, no. 1 (2005): 89-93.
Katsambas A et al., “Hyperpigmentation and melasma treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Aldahan AS et al., “Topical treatments for melasma and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Passeron T et al., “Melasma pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Draelos ZD et al., “Efficacy of natural ingredients in anti-pigmentation and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Sivamani RK et al., “Natural alternatives for treating hyperpigmentation and skin inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Nistico SP et al., “Efficacy of botanical formulations for managing hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Baumann L et al., “Chemical peels: An evidence-based review.” American Journal of Clinical Dermatology 10, no. 6 (2009): 297-306.
Nistico SP et al., “Topical retinoids and inflammation: A review.” Dermatologic Therapy 34, no. 2 (2021): e14830.
Alvarez OM et al., “Botanical extracts for skin lightening: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Grimes PE et al., “Histologic changes in hyperpigmented skin.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Boonchai W et al., “Post-inflammatory hyperpigmentation: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Pekarek B et al., “Cryotherapy versus curettage for seborrheic keratosis: A comparative study.” Journal of Dermatologic Surgery 31, no. 10 (2005): 1316-1320.
Sardana K et al., “Rebound pigmentation and its management in hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Handog EB et al., “Challenges in the management of hyperpigmentation: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in hyperpigmentation management.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Kraft JN et al., “The role of inflammation in hyperpigmentation and its management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Considerations with Mainstream Treatments
Laser Therapy


Chemical Peels


Topical Treatments


We're here to help you manage your skin concerns.
Sardana K et al., “Rebound pigmentation and its management in hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Goldberg DJ et al., “Pigment-safe laser treatments for benign skin lesions.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Dika E et al., “Laser treatment for benign melanocytic nevi: A review.” Lasers in Medical Science 33, no. 4 (2018): 853-861.
Rodriguez CI et al., “Role of oxidative stress in hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Passeron T et al., “Melasma pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and melasma treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Gupta AK et al., “Chemical peels for melasma in dark-skinned patients.” Dermatologic Surgery 25, no. 4 (1999): 243-248.
Baumann L et al., “Chemical peels: An evidence-based review.” American Journal of Clinical Dermatology 10, no. 6 (2009): 297-306.
Aldahan AS et al., “Topical treatments for melasma and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Grimes PE et al., “Histologic changes in hyperpigmented skin.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Handog EB et al., “Challenges in the management of hyperpigmentation: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24. Sivamani RK et al., “Natural alternatives for treating hyperpigmentation and skin inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Lim JT et al., “Sun protection and prevention of hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Briganti S et al., “Melanin: What is it and how is it produced?” International Journal of Cosmetic Science 25, no. 6 (2003): 279-289.
Hassim Z et al., “Hormonal influences on hyperpigmentation: A comprehensive review.” International Journal of Women’s Dermatology 6, no. 2 (2020): 73-82.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in hyperpigmentation management.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Draelos ZD et al., “Efficacy of natural ingredients in anti-pigmentation and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Hassim Z et al., “Management of exogenous ochronosis caused by topical hydroquinone.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Olumide YM et al., “Exogenous ochronosis in black skin: A report of 22 cases.” International Journal of Dermatology 47, no. 3 (2008): 344-350.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.