What is PhytoLift
How It Works
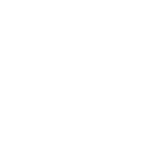
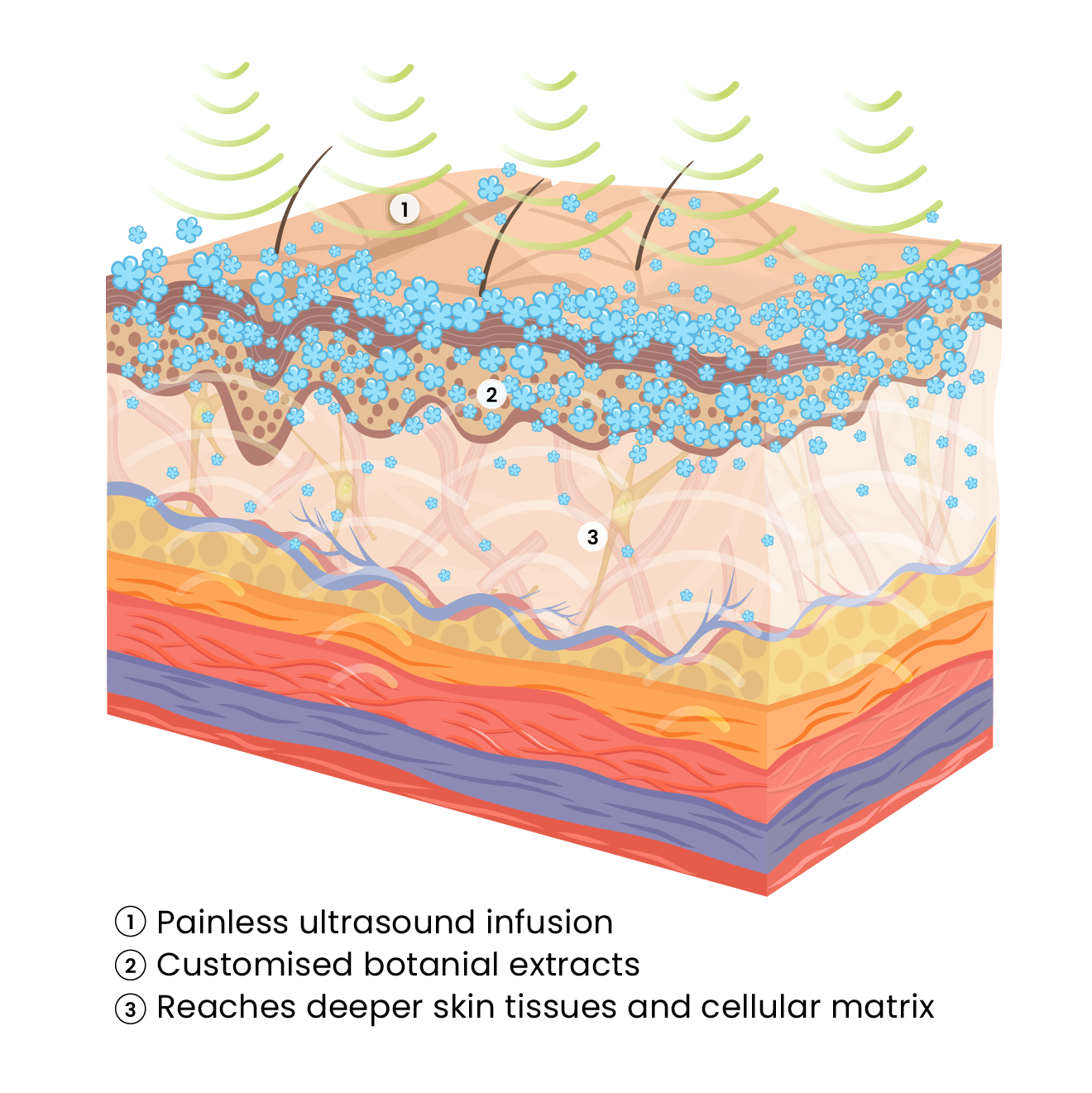
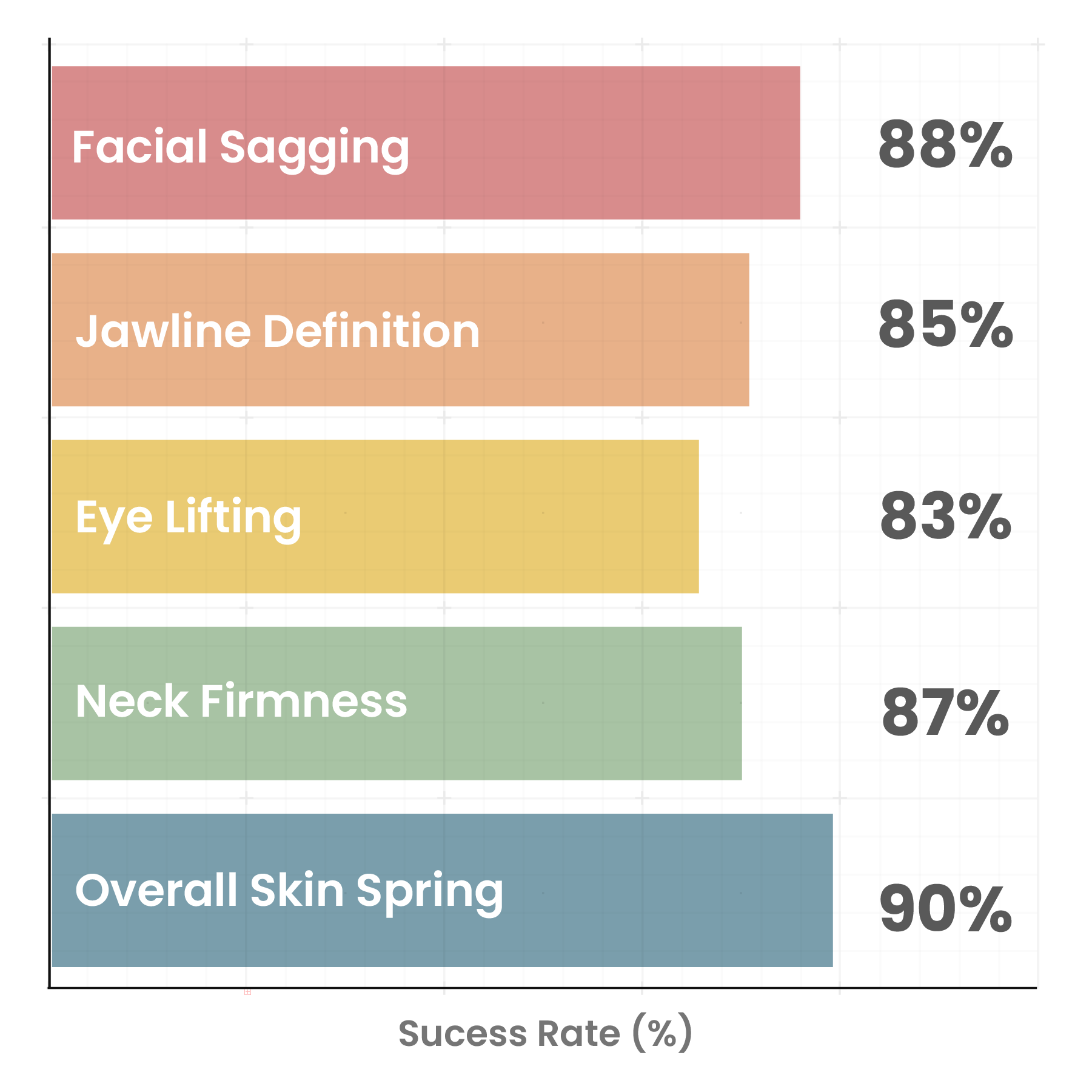
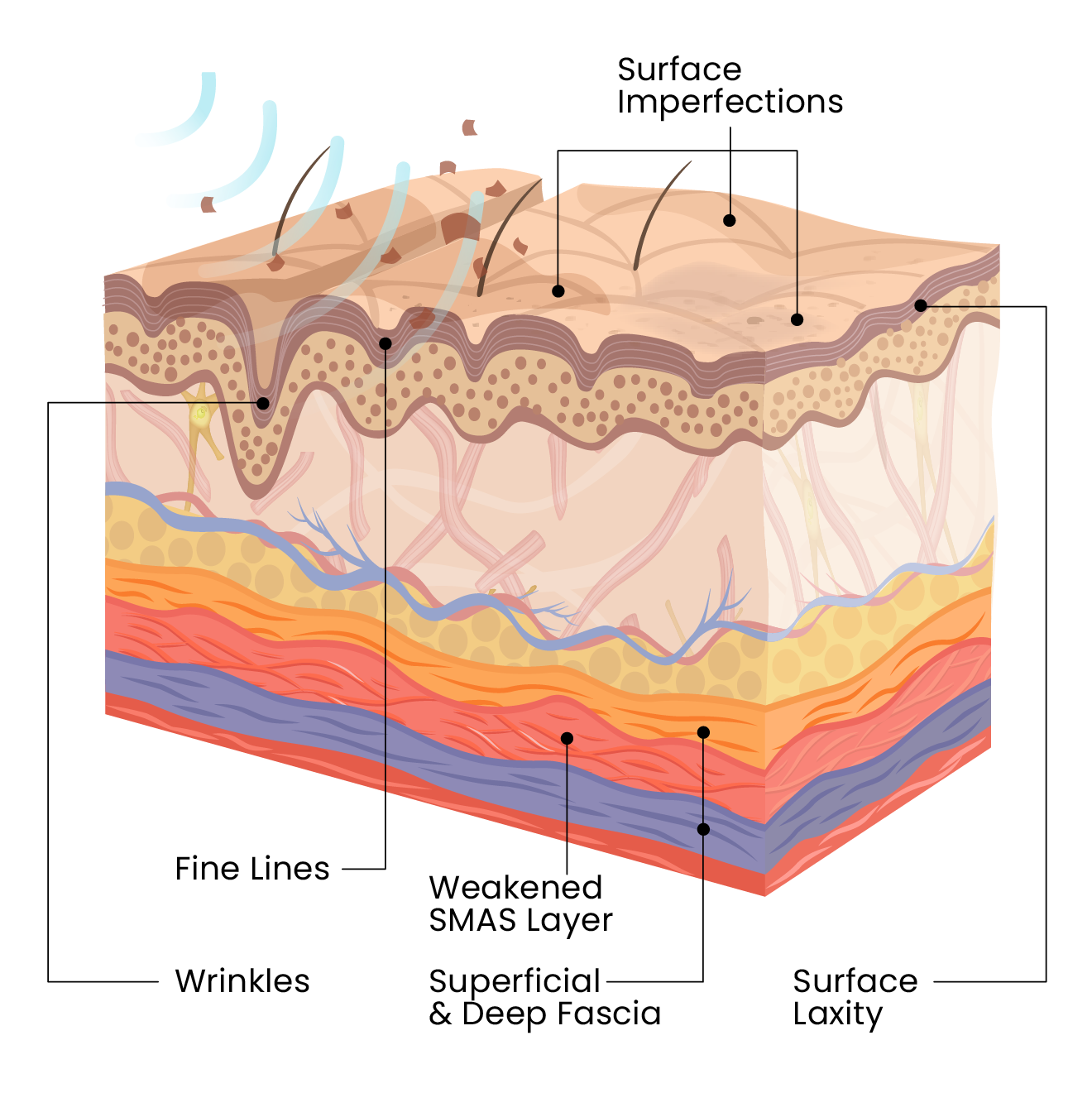
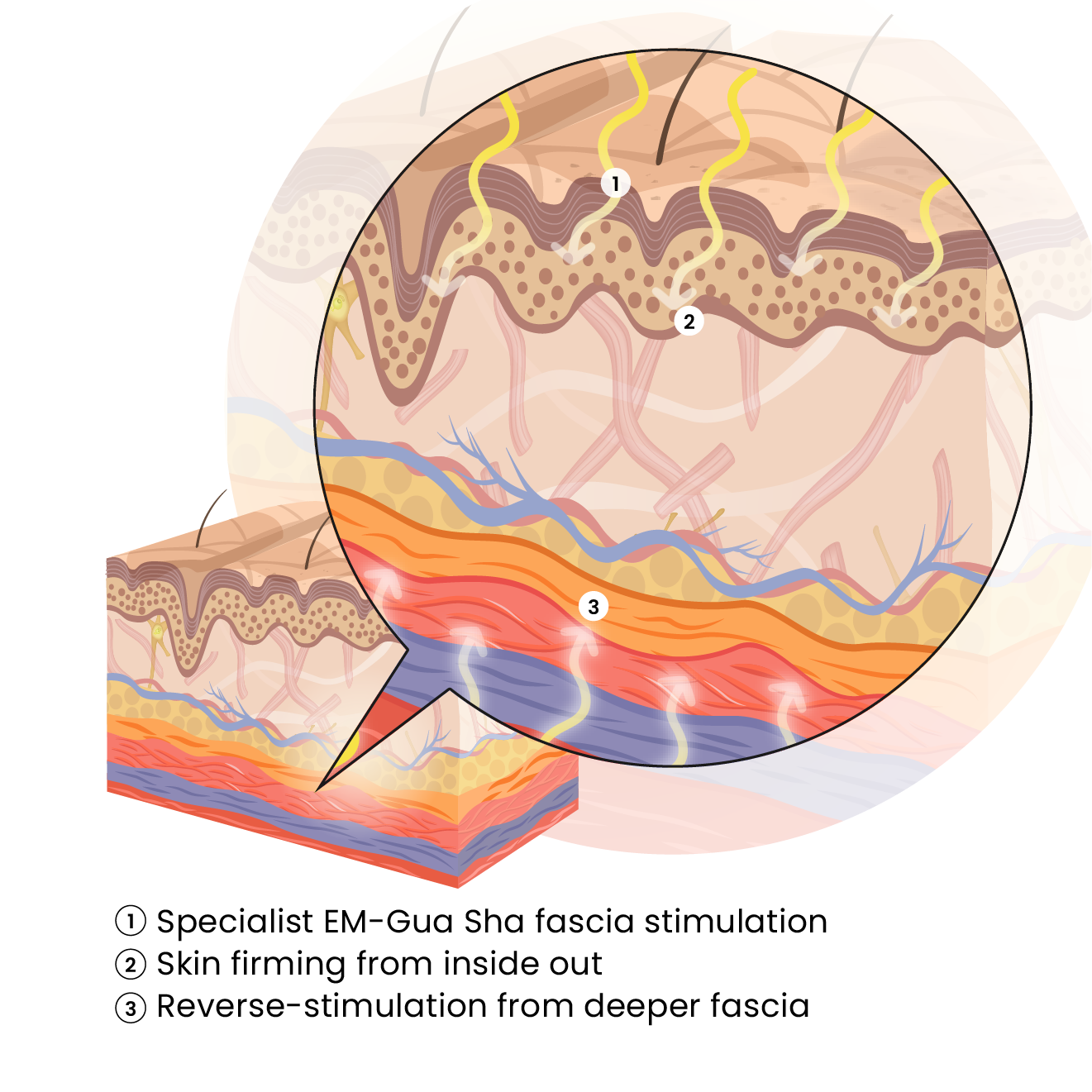
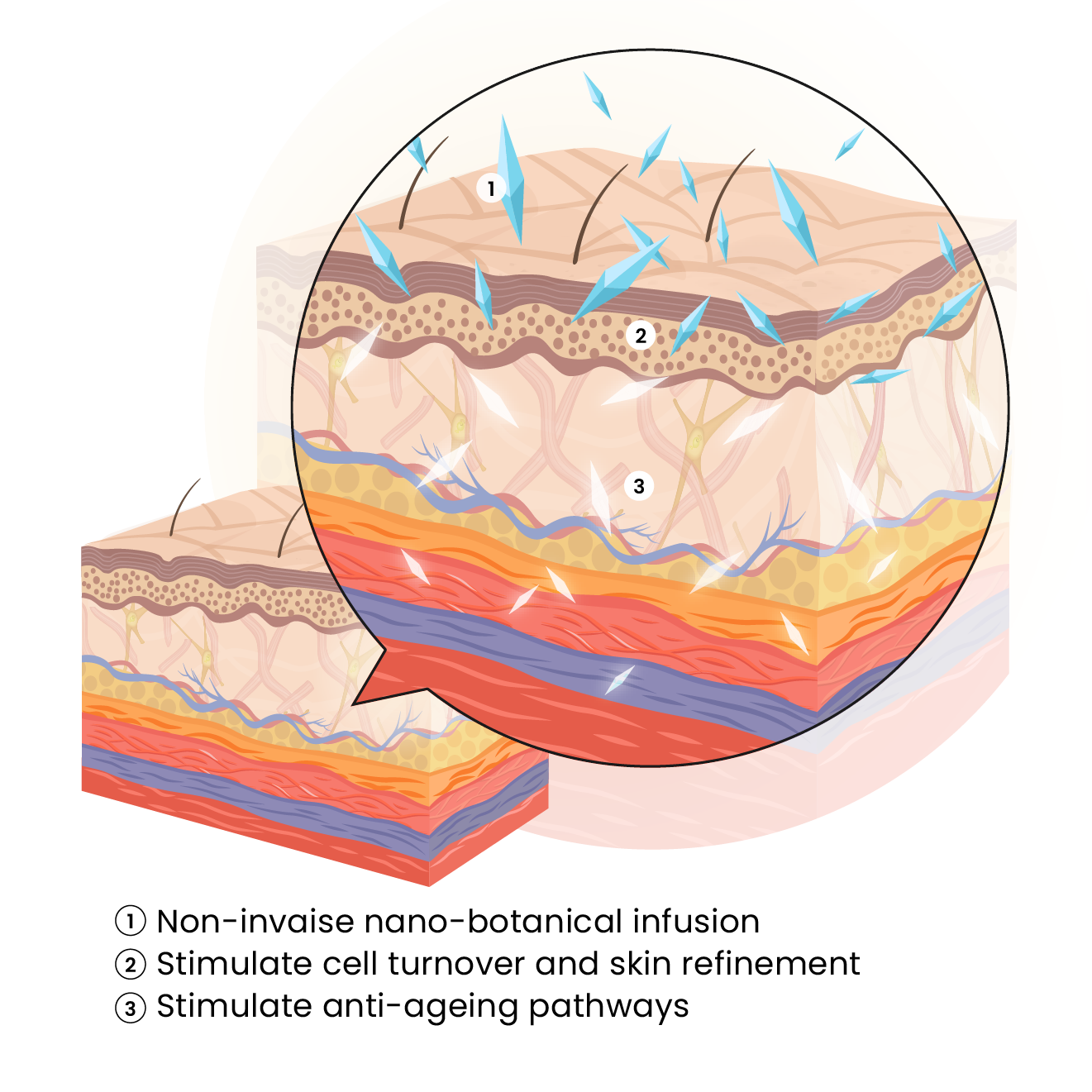
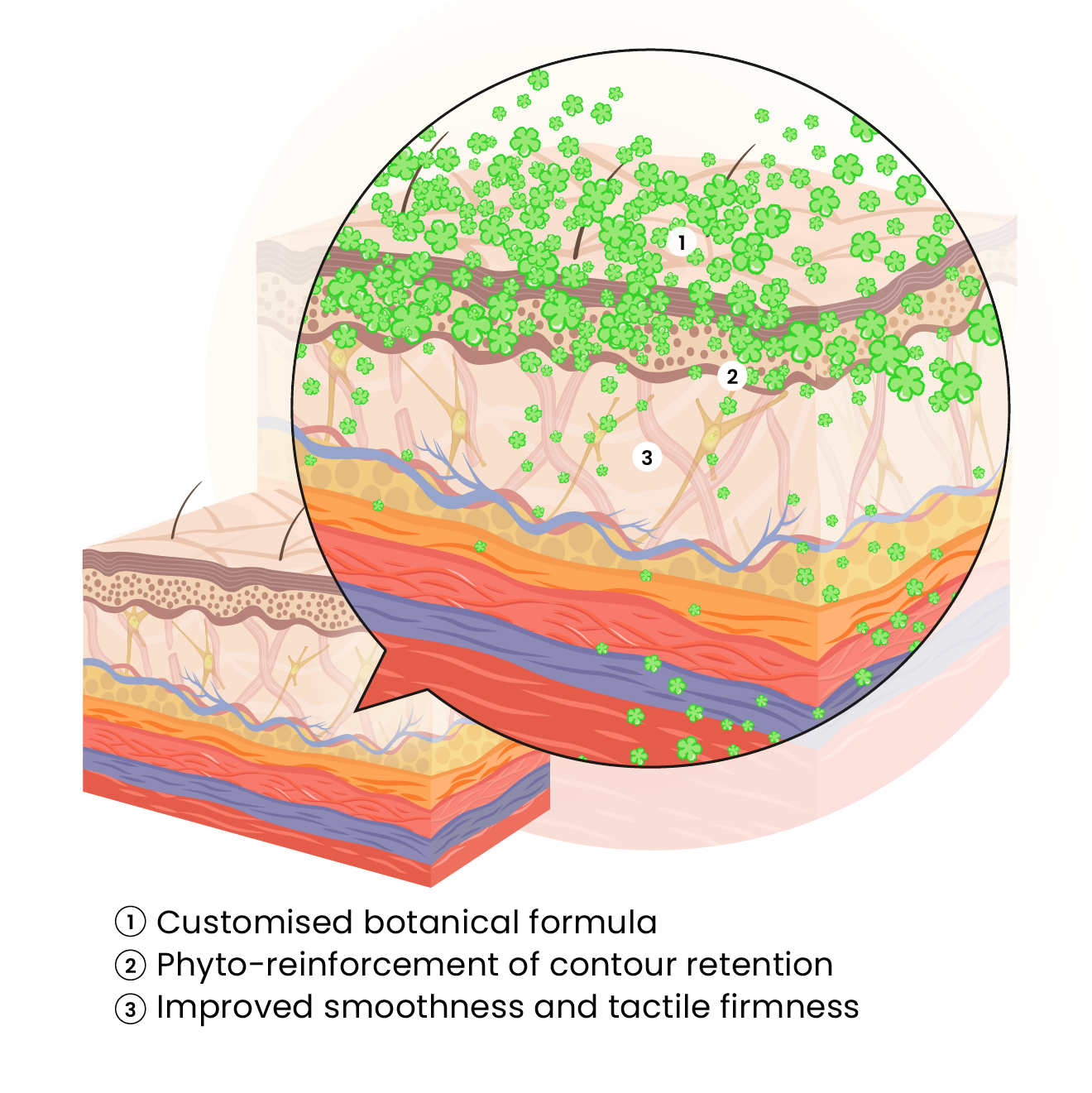
PhytoLift™ uses in-house reconditioning and non-invasive methodologies to lift sagging skin, tone muscles, and restore definition. Each session targets fascia and dermal support for visible firmness without trauma or downtime.


Who Is It For
How Is It Different
| Mainstream Methods | PhytoLift™ Approach |
|---|---|
| Injections that distort proportions or risk nerve disruption | Harmonious lifting aligned with your skin and muscle structure |
| Over-tightening from surface-only treatments | Deep renewal of fascia, muscle tone, and collagen network |
| Loss of structural facial fat caused by aggressive, non-invasive energy treatments | Fascia and muscle activation with zero risk of fat layer depletion |
| Painful thread lifts, excessive fillers, or invasive surgery | Non-invasive fascia and muscle reactivation without trauma |
| Risk of stiffness or loss of natural facial mobility | Restores tone and expression through active reconditioning |
| Temporary plumping with bruising and painful downtime | Natural lift without swelling, bruising, or surface damage |
| Generic RF or energy facials with limited personalisation | Specialist-led, fascia-targeted protocol with in-house methods |
| Frequent touch-ups needed as effects deplete quickly to baseline | Residual lift builds progressively by nurturing your cellular matrix and structural integrity |
Reclaim Your Facial Definition ✧
Baumann L et al., “Skin ageing and its treatment.” Journal of the American Academy of Dermatology 60, no. 4 (2009): 532-543.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Sadick NS et al., “The impact of collagen production on skin ageing.” Journal of Clinical and Aesthetic Dermatology 13, no. 6 (2020): 18-25.
Sivamani RK et al., “Natural alternatives for treating aging skin and inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Passeron T et al., “Melasma and aging: Pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and aging treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Alvarez OM et al., “Botanical extracts for skin lightening and anti-aging: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Boonchai W et al., “Post-inflammatory hyperpigmentation and aging: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Grimes PE et al., “Histologic changes in hyperpigmented skin.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Nistico SP et al., “Efficacy of botanical formulations for managing aging and hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Draelos ZD et al., “Efficacy of natural ingredients in anti-aging and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Hasson A et al., “Long-term effects of injectable fillers: Complications and management.” Journal of Clinical and Aesthetic Dermatology 13, no. 6 (2020): 18-25.
Sadick NS et al., “Volume loss and filler fatigue: Understanding the longevity of injectable fillers.” Dermatologic Surgery 43, no. 6 (2017): 848-855.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Dika E et al., “Laser treatment for benign melanocytic nevi: A review.” Lasers in Medical Science 33, no. 4 (2018): 853-861.
Narins RS et al., “Safety of hyaluronic acid fillers: A comprehensive review.” Dermatologic Surgery 37, no. 10 (2011): 1697-1705.
Matarasso SL et al., “Complications of soft tissue augmentation: Prevention and management.” Journal of the American Academy of Dermatology 66, no. 1 (2012): 11-22.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Fabi SG et al., “Collagen stimulation and neoformation: A review of the science behind dermal fillers.” Journal of Drugs in Dermatology 13, no. 9 (2014): 1044-1052.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Boonchai W et al., “Post-inflammatory hyperpigmentation: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Bolognia JL et al., “Complications of lasers and light-based devices in dermatology.” Dermatologic Therapy 26, no. 5 (2013): 332-343.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Baumann L et al., “Chemical peels: An evidence-based review.” American Journal of Clinical Dermatology 10, no. 6 (2009): 297-306.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Narins RS et al., “Long-term complications of injectable soft tissue fillers: A review.” Dermatologic Surgery 34, no. 12 (2008): 1574-1579.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Hassim Z et al., “Hormonal influences on aging and hyperpigmentation: A comprehensive review.” International Journal of Women’s Dermatology 6, no. 2 (2020): 73-82.
Briganti S et al., “Melanin: What is it and how is it produced?” International Journal of Cosmetic Science 25, no. 6 (2003): 279-289.
Solano F, “Melanins: Skin pigments and much more—types, structural models, biological functions, and formation routes.” New Journal of Science 2014 (2014): 1-28.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Draelos ZD et al., “Efficacy of natural ingredients in anti-aging and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Alvarez OM et al., “Botanical extracts for skin lightening and anti-aging: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Nistico SP et al., “Efficacy of botanical formulations for managing aging and hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Sivamani RK et al., “Natural alternatives for treating aging skin and inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Passeron T et al., “Melasma and aging: Pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and aging treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Boonchai W et al., “Post-inflammatory hyperpigmentation and aging: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
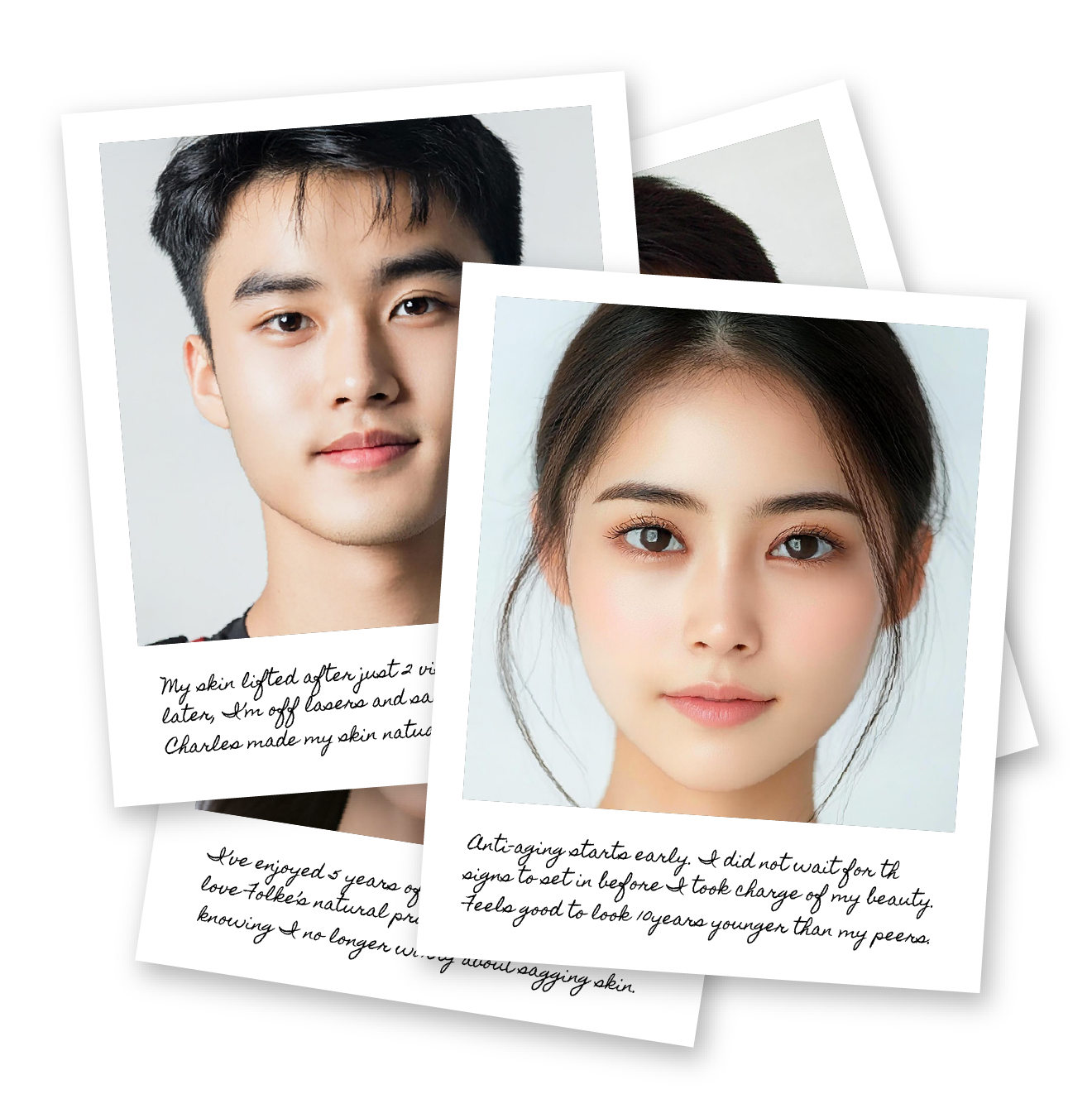
Before & After

Sagging cheeks, jowls, and a blunted jawline distort facial balance, reducing harmony, definition, and structure across the mid-lower face.

Cheeks appear elevated and the jawline reshaped. Facial contours look firmer, more sculpted, and visibly lifted.

Laxity in the neck shows up as horizontal folds, loose skin, and early “tech neck” lines that worsen with posture, ageing, and muscle weakening.

Skin around the neck tightens with greater tension and tone. Horizontal lines soften and posture appears more upright.

Overly relaxed eyelids, sagging brows, and puffiness create a sunken, tired expression that makes the face look older and more fatigued than it is.
Brows lift, lids open, and puffiness reduces visibly. Eye area appears more alert, refreshed, and youthful without downtime.

Skin deflates after childbirth or major weight loss, leaving cheeks, jaw, and neck with looseness, poor tension, and visible structural collapse.

Skin regains compactness and firmness without needles. Contours appear more supported, and toned across multiple zones.